This one's for the girls-think pink & get checked.
Breast Cancer Awareness Month: facts, myths and prevention.
It’s October and I noticed that last Friday everyone was wearing pink at work, I naively asked, “Did I miss the memo? What’s going on?”
Everyone’s showing up for breast cancer awareness month. Everything’s fine now, I've neatly folded my pink shirt for tomorrow morning. But with pink ribbons everywhere and pink branding on face creams and body washes, I wondered where the proceeds for all these sales were going. “Pinkwashing,” is a term coined by Breast Cancer Action in an effort to call out companies that sell products related to breast cancer awareness.
Breast Cancer Action runs its “Think Before You Pink” campaign annually to call out companies who “pinkwash,” or produce pink-ribboned adorned products from carcinogenic material “while raising millions to feed their own bottom line.”
The campaign is designed to improve awareness of companies raising large sums of money with only a small portion going to breast cancer research, with hopes of people donating in the most effective way. Before buying the pink product, research where the proceeds are going and if there are other organizations that might have a greater impact.
This month can mean many things to many people; some wear pink in celebration, some quietly reflect, some may experience grief, and others might feel unseen or misunderstood. Whatever your feelings are towards this month, all are valid. And despite the lack of transparency from big companies’ profits and donations, Breast Cancer Awareness Month is also a month to encourage screening and prevention.
I grew up hearing about my mom’s side of the family and their history of breast cancer; 3 of my maternal grandmother’s sisters and 1 brother had a diagnosis in their lifetime and went through treatment, and my grandma had some sort of preventative treatment.
This was a story I grew to re-tell all my new OB/GYNs as I moved from city to city, followed by an “it’s okay, nothing to worry about now.” With time, I’ve found peace with knowing that since my mom (my first-degree relative) is okay, I am too-at least that’s what I gathered from my past two doctors.
Breast cancer is the most common cancer excluding some skin cancers which are not required to be reported to cancer registries; it is also the second most common cause of death from cancer among women, following lung cancer.
In the course of their lifetime, 1 in 8 women will have an invasive breast cancer diagnosis. Mortality has decreased since the 1970s thanks to earlier detection through breast cancer screenings and advancements in adjuvant therapy (also known as “helper therapy,” which targets cells that primary treatment did not destroy, and reduces the risk of that cancer returning.) There is now a 90.8% 5-year relative survival rate, meaning the % of patients who would be expected to survive the effects of their cancer 5 years after diagnosis is quite high.
Though more common in women, men can also have breast cancer. In 2023 around 2,800 men will be diagnosed with breast cancer, compared to 297,790 new cases in women according to the American Cancer Society.
There is a higher risk of incidence in non-Hispanic white women, followed closely by non-Hispanic black women however, black women have the highest breast cancer death rate with 28.4 deaths per 100,000. Disparities are attributed to socioeconomic status and access to healthcare, lower rates of breastfeeding, and genetics.
What is it?
Breast cancer is a group of diseases in which cells in breast tissue change and divide uncontrolled, typically resulting in a lump or mass. Most common physical signs include a painless lump, and swelling or lumps in underarm lymph nodes. Less common signs include redness, swelling, or thickening of the skin, and nipple changes such as scaliness or spontaneous discharge. It’s important to discuss these changes with your doctor as soon as you notice them.
There are many types of breast cancers, classified by the specific cells in the breast that become cancer. Most are adenocarcinomas, or tumors that start at the epithelial cells in the milk ducts or lobules (glands in the breast that make milk). Further categorization refers to whether the cancer has spread or not. To go into detail about each type would go beyond the scope of today’s piece, but here is some more detailed information, as well as here, for those interested.
What are the types of breast cancer screening?
The United States Preventive Task Force encourages women ages 50-74 who are at average risk for breast cancer to get a mammogram every 2 years. Women below 50 should talk to their physicians about when to get screened and how often, taking into account the risks and benefits of screening tests.
There are various screening tests available to aid in the early detection and confirmation of a breast cancer diagnosis.
Mammogram: an X-ray of the breast and is usually the best way to detect changes such as tumors, lumps, and other abnormalities.
Breast Magnetic Resonance Imaging (MRI): uses magnets and radio waves to take pictures, and is used alongside mammograms to screen and diagnose women at higher risk.
Clinical breast exams: performed by doctors and nurses who use their hands to feel for any lumps or changes to the breast during an appointment.
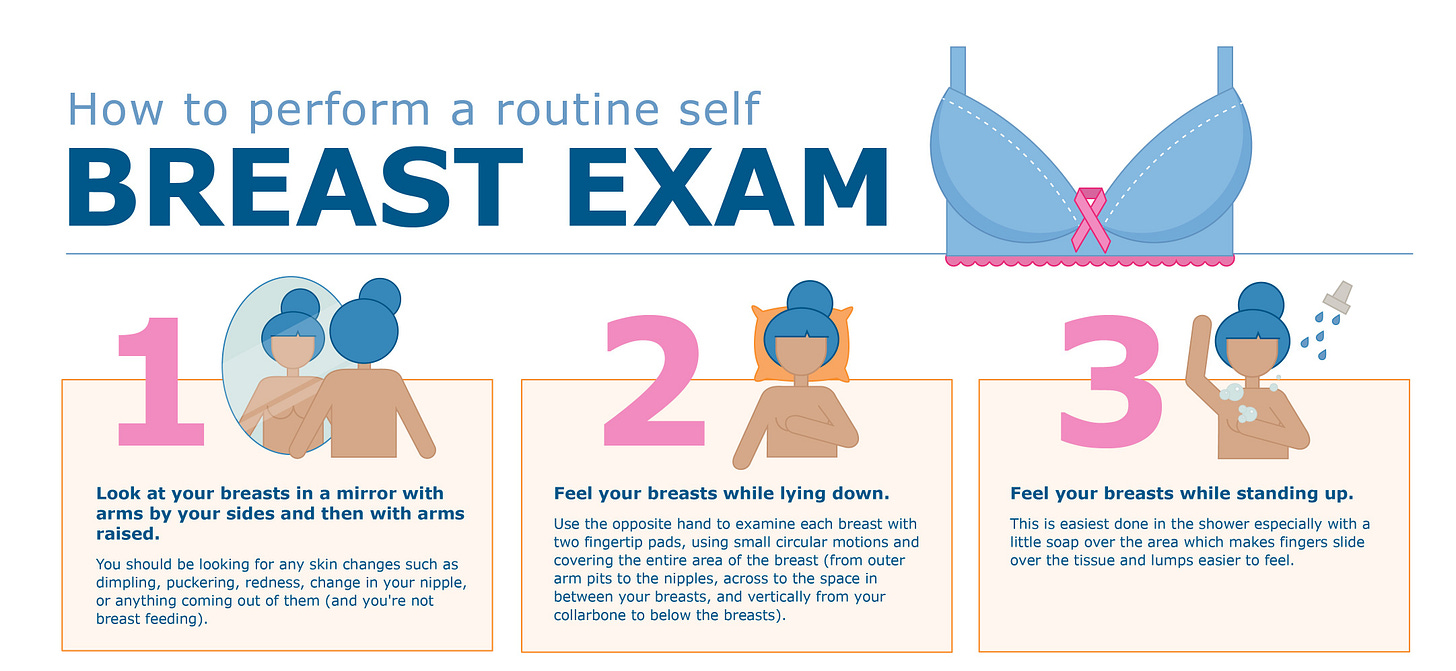
Breast self-exam: is a similar exam done by yourself at home. It is important to be familiar with what your breasts normally look and feel like, so you can be aware of any changes that might arise during a breast self-exam, for more info click here for a “how-to” guide.
What are some risk factors?
Studies show that the risk of breast cancer diagnosis is due to many factors, the main ones are A) being a woman and B) older age. So yeah, basically getting checked and being familiarized with your breasts is important for all women, especially those above the age of 50 when most breast cancers are usually detected.
It is a complex disease that is affected by genetics, lifestyle, and environmental factors. Some risk factors are modifiable, meaning you can do something about them to lower your risk, others are not.
Having risk factors does not mean you will have a breast cancer diagnosis, they indicate an increased likelihood but are not definitive predictors; many people with several risk factors might never develop cancer, while others with no apparent risk factors might.
3 Non-Modifiable Risk Factors:
Genetic mutations: Inherited mutations in the BRCA1, BRCA2, and other genes can significantly increase the risk of breast cancer.
Menstrual history: Women who started menstruating at an early age (<12 years old) and women who experienced menopause at a later time in life may have a greater risk; the proposed mechanism is that being exposed to estrogen for a long time increases risk.
Family history of breast or ovarian cancer in a first-degree relative (mother, sister, daughter), or personal history of breast cancer or other breast-related diseases
3 Modifiable Risk Factors:
Leading a sedentary lifestyle: It’s especially true for women past menopause that regular physical activity reduces breast cancer risk.
Smoking/drinking alcohol: Smoking may lead to genetic mutations and can increase the risk of disease, especially for girls who smoke during adolescence or before they start menstruating. Alcohol seems to increase risk in a dose-dependent way, meaning the more you drink the higher the risk, not only for breast cancer but for other types of cancer as well.
Hormone replacement therapy and oral contraceptives: Menopausal hormonal therapy that has mixed hormones (both estrogen and progesterone) may increase the risk of disease. Oral contraceptives (OCPs) lead to a slight increase in risk when compared to women who have never used them, but this risk seems to decrease after 10 years of stopping the pill. It’s worth noting that OCPs can also lead to a decreased risk of other ovarian and uterine cancers.
What are some preventive measures I can take?
Breastfeeding: Breastfeeding may decrease the risk of breast cancer if continued for 1+ years, if you are having difficulties try to contact a lactation consultant for help. If this is not feasible for you, no worries, it’s just one of many things you can do, remember, fed is best!
Genetic counseling and testing: If you have immediate family that has had or has breast cancer, you can always opt for testing. Talk to your doctor to see if this is available to you, most likely they will do a risk assessment first to determine if further testing is needed wherein they will look if the BRCA1 and BRCA2 genes were inherited.
Physical activity: Keep it movin’! There is strong evidence to suggest that regular physical activity reduces disease risk through proposed mechanisms of lowering inflammation, weight, and hormone levels; choose an activity you like and try to follow the recommended ~150-300 minutes of moderate-intensity or 75 to 150 minutes of vigorous-intensity activity each week.
Follow a balanced, healthy dietary pattern: Nutrition science is ever-changing, and no single food or diet can prevent a breast cancer diagnosis, but following a dietary pattern rich in plant-based foods, low in red meat and refined carbs may help decrease risk. A diet that’s high in calcium (think leafy greens, low-fat dairy foods), carotenoids (the red/orange pigment in fruits and veggies such as in carrots and squash), and cruciferous vegetables (think broccoli, cabbage, kale) have also been thought to decrease risk. Limiting alcohol to 1 glass or less, or abstaining, as mentioned can also lower risk of disease.
Common Myths:
“Big boobs mean you have a greater chance of getting breast cancer”
False, breast density but not breast size is considered a risk factor. Dense breast tissue can also make it harder to see tumors on mammograms.
“Having your phone inside your bra will lead to cancer”
Nop, no studies have shown this to be true, though I’d say it doesn’t sound like the most comfortable place to have your phone in…
“Breast pain means you have breast cancer”
Well, not really, it might mean you’re getting your period, or are pregnant, or a myriad of other things, but pain is not usually a sign of breast cancer. If you are experiencing consistent or new breast pain talk to your doctor to discuss causes/solutions.
“Using deodorant increases your chance of getting breast cancer”
Not enough science to back that claim up TBH. However, using aluminum-containing deodorant on days you have a mammogram is not encouraged. Although it does not increase the risk of a diagnosis, aluminum does show up as white specks on a mammogram, which can be confused for microcalcifications to the breast.
If you are concerned about your risk of breast cancer due to multiple risk factors, it's a good idea to consult with a healthcare provider or a genetic counselor.
They can provide you with personalized risk assessments, guidance on risk reduction strategies, and recommendations for appropriate screenings or genetic testing, should they be warranted.
Being proactive about your breast health and maintaining a healthy lifestyle can help mitigate some of the risks associated with breast cancer.
“Pink together, stronger forever”
Keep chewin’ :)








Excelente información! Love you 😘